

Toxoplasma gondii. Toxoplasma gondii (tŏk'sə-plāz'mə gŏn'dē-ī') is an obligate, intracellular, parasitic protozoan that causes the disease toxoplasmosis.[1] Found worldwide, T. gondii is capable of infecting virtually all warm-blooded animals.[2] In humans, it is one of the most common parasites;[3] serological studies estimate that up to a third of the global population has been exposed to and may be chronically infected with T. gondii, although infection rates differ significantly from country to country.[4] Although mild, flu-like symptoms occasionally occur during the first few weeks following exposure, infection with T. gondii generally produces no symptoms in healthy human adults.[5][6] However, in infants, HIV/AIDS patients, and others with weakened immunity, infection can cause serious and occasionally fatal illness (toxoplasmosis).[5][6] Infection in humans and other warm-blooded animals can occur Dividing T. gondii parasites Diagram of T. gondii structure Lifecycle[edit]

Chlorpromazine - PubMed Health. Chlorpromazine. Chlorpromazine (as chlorpromazine hydrochloride, abbreviated CPZ; marketed in the United States as Thorazine and elsewhere as Largactil or Megaphen) is a dopamine antagonist of the typical antipsychotic class of medications possessing additional antiadrenergic, antiserotonergic, anticholinergic and antihistaminergic properties used to treat schizophrenia.[3][4] First synthesized on December 11, 1950, chlorpromazine was the first drug developed with specific antipsychotic action, and would serve as the prototype for the phenothiazine class of drugs, which later grew to comprise several other agents.
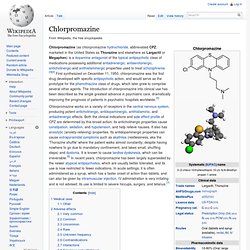
The introduction of chlorpromazine into clinical use has been described as the single greatest advance in psychiatric care, dramatically improving the prognosis of patients in psychiatric hospitals worldwide.[5] Chlorpromazine works on a variety of receptors in the central nervous system, producing potent anticholinergic, antidopaminergic, antihistaminic, and antiadrenergic effects. Fatal familial insomnia. Fatal familial insomnia (FFI) is an extremely rare autosomal dominant inherited prion disease of the brain.

It is almost always caused by a mutation to the protein PrPC, but can also develop spontaneously in patients with a non-inherited mutation variant called sporadic fatal insomnia (sFI). FFI has no known cure and involves progressively worsening insomnia, which leads to hallucinations, delirium, and confusional states like that of dementia.[1] The average survival span for patients diagnosed with FFI after the onset of symptoms is 18 months.[1] The mutated protein, called PrPSc, has been found in just 40 families worldwide, affecting about 100 people; if only one parent has the gene, the offspring have a 50% risk of inheriting it and developing the disease. With onset usually around middle age, it is essential that a potential patient be tested if they wish to avoid passing FFI on to their children.
The first recorded case was an Italian man, who died in Venice in 1765.[2]