

MPR 09.12 Admission Hyperglycemia Predicts Mortality in COVID 19 Clinical Advisor. Thromb Haemos Frecuencia de tromboembolismo en COVID 10. Features, Evaluation and Treatment Coronavirus (COVID-19) - StatPearls - NCBI Bookshelf. 'How is this possible?' Researchers grapple with Covid-19's mysterious mechanism. Respiratory physician Dr David Darley says something peculiar happens to a small group of Covid-19 patients on day seven of their symptoms.
“Up until the end of that first week, they’re stable,” says Darley, a doctor with Sydney’s St Vincent’s Hospital. “And then suddenly, they have this hyper-inflammatory response. The proteins involved in that inflammation start circulating in the body at high levels.” In these patients, the lungs begin to struggle. Blood pressure lowers. “I think what is evolving is a very specific set of stages of disease and for some reason, not everyone goes through all of the stages,” Darley says. But there is no way of knowing which patients will be affected by the most severe symptoms. “It would help clinicians predict what stage patients are at and maybe even if they will progress to the next stage of disease,” he said. HARVARD_EDU 24/07/20 How COVID-19 causes smell loss. Temporary loss of smell, or anosmia, is the main neurological symptom and one of the earliest and most commonly reported indicators of COVID-19.
Studies suggest it better predicts the disease than other well-known symptoms such as fever and cough, but the underlying mechanisms for loss of smell in patients with COVID-19 have been unclear. Now, an international team of researchers led by neuroscientists at Harvard Medical School has identified the olfactory cell types in the upper nasal cavity most vulnerable to infection by SARS-CoV-2, the virus that causes COVID-19. Surprisingly, sensory neurons that detect and transmit the sense of smell to the brain are not among the vulnerable cell types. Reporting in Science Advances on July 24, the research team found that olfactory sensory neurons do not express the gene that encodes the ACE2 receptor protein, which SARS-CoV-2 uses to enter human cells.
Pinpointing vulnerability. Jama 09.07 Síntomas persistentes de COVID. Coronavirus Infections—More Than Just the Common Cold. Human coronaviruses (HCoVs) have long been considered inconsequential pathogens, causing the “common cold” in otherwise healthy people.
However, in the 21st century, 2 highly pathogenic HCoVs—severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV)—emerged from animal reservoirs to cause global epidemics with alarming morbidity and mortality. In December 2019, yet another pathogenic HCoV, 2019 novel coronavirus (2019-nCoV), was recognized in Wuhan, China, and has caused serious illness and death. The ultimate scope and effect of this outbreak is unclear at present as the situation is rapidly evolving. COVID-19, not ‘just a flu’ – News. The avalanche of coronavirus infections in the current pandemic has been accompanied by a similar avalanche of information, making it hard to sift reliable news from the noise, according to Professor Mike Lee and Dr Sebastian Duchene in their The Conversation article (reproduced below, originally published on 17 March.)
Among the most crucial questions is: how deadly is the SARS-CoV-2 virus? First things first: contrary to some reports, there is no evidence the virus has evolved a new, deadlier strain since it emerged in late 2019. Think a 'mild' case of Covid-19 doesn’t sound so bad? Think again. Conventional wisdom suggests that when a sickness is mild, it’s not too much to worry about.

But if you’re taking comfort in World Health Organization reports that over 80% of global Covid-19 cases are mild or asymptomatic, think again. MPR 11.12 Systemic Analysis of the Hallmarks of Advanced COVID 19 Pathology Infectious Disease Advisor. COVID-19: The immune system can fight back. Melbourne researchers have mapped immune responses from one of Australia’s first novel coronavirus (COVID-19) patients, showing the body’s ability to fight the virus and recover from the infection.
Researchers at the Peter Doherty Institute for Infection and Immunity (Doherty Institute) – a joint venture between the University of Melbourne and the Royal Melbourne hospital – were able to test blood samples at four different time points in an otherwise healthy woman in her 40s, who presented with COVID-19 and had mild-to-moderate symptoms requiring hospital admission. Published today in Nature Medicine is a detailed report of how the patient’s immune system responded to the virus. One of the authors on the paper, research fellow Dr Oanh Nguyen said this was the first time that broad immune responses to COVID-19 have been reported. CDC 24.07 Duración de los síntomas y vuelta a la vida normal. Mark W.

Tenforde, MD, PhD1; Sara S. Kim, MPH1,2; Christopher J. Lindsell, PhD3; Erica Billig Rose, PhD1; Nathan I. Shapiro, MD4; D. Clark Files, MD5; Kevin W. View suggested citation Summary. Doctor's Note: Why are young people dying from coronavirus? How does coronavirus kill? Clinicians trace a ferocious rampage through the body, from brain to toes. Science’s COVID-19 reporting is supported by the Pulitzer Center.

On rounds in a 20-bed intensive care unit one recent day, physician Joshua Denson assessed two patients with seizures, many with respiratory failure and others whose kidneys were on a dangerous downhill slide. Days earlier, his rounds had been interrupted as his team tried, and failed, to resuscitate a young woman whose heart had stopped. All shared one thing, says Denson, a pulmonary and critical care physician at the Tulane University School of Medicine. “They are all COVID positive.” As the number of confirmed cases of COVID-19 surges past 2.2 million globally and deaths surpass 150,000, clinicians and pathologists are struggling to understand the damage wrought by the coronavirus as it tears through the body.
Understanding the rampage could help the doctors on the front lines treat the fraction of infected people who become desperately and sometimes mysteriously ill. Related story The infection begins An invader’s impact. What the coronavirus does to your body that makes it so deadly. COVID-19 is caused by a coronavirus called SARS-CoV-2.
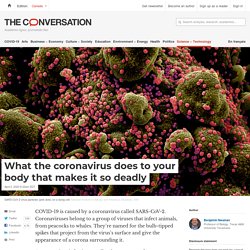
Coronaviruses belong to a group of viruses that infect animals, from peacocks to whales. They’re named for the bulb-tipped spikes that project from the virus’s surface and give the appearance of a corona surrounding it. The paths of destruction - How SARS-CoV-2 causes disease and death in covid-19. Editor’s note: Some of our covid-19 coverage is free for readers of The Economist Today, our daily newsletter.

For more stories and our pandemic tracker, see our coronavirus hub THE FIRST SET of lungs felt like rubber, says Rainer Claus, so damaged that it was impossible to imagine how any amount of oxygen could get through them. The lungs in the rest of the ten covid-19 victims that he and his colleagues at the University Medical Centre Augsburg, in Germany, autopsied in early April were in similarly awful condition. This has been, for the most part, the story around the world. Coronavirus symptoms fall into six different groupings, study finds. Symptoms of Covid-19 appear to fall into six different groupings, researchers have revealed, in work they say could help to predict whether a patient will end up needing a ventilator or other breathing support. The team say the findings could give healthcare providers several days advanced warning of demand for hospital care and respiratory support.
But it could also help flag patients at risk of becoming seriously ill, meaning home support, such as an oxygen meter or nurse visits, could be provided so that any deterioration is spotted quickly and hospital attendance is prompt. Here's how your body gains immunity to coronavirus. As the daughter of an air force officer and a nurse, I am fascinated by defence systems. There is none more impressive than the human immune system, equipped as it is with a rich arsenal to defend against different types of pathogen. Viruses have evolved to trick, bypass and evade these defences. Global Consortium Study of Neurological Dysfunction in COVID-19 (GCS-NeuroCOVID): Study Design and Rationale. COVID y deterioro cognitivo J Psy. What Does Covid-19 Do to Your Brain? Warning of serious brain disorders in people with mild coronavirus symptoms.
Doctors may be missing signs of serious and potentially fatal brain disorders triggered by coronavirus, as they emerge in mildly affected or recovering patients, scientists have warned. Neurologists are on Wednesday publishing details of more than 40 UK Covid-19 patients whose complications ranged from brain inflammation and delirium to nerve damage and stroke. In some cases, the neurological problem was the patient’s first and main symptom. The cases, published in the journal Brain, revealed a rise in a life-threatening condition called acute disseminated encephalomyelitis (Adem), as the first wave of infections swept through Britain. At UCL’s Institute of Neurology, Adem cases rose from one a month before the pandemic to two or three per week in April and May. How Covid-19 can damage the brain - BBC Future. In France, Helms knows better than almost anyone how intense the neurological impacts can be.
We needed to delay her interview with the BBC after one of her Covid-19 patients – who was discharged from the hospital two months ago, but is still suffering from viral fatigue and severe depression – required urgent consultation for suicidal risk. And that patient is not unique – she has seen many people in similar states of distress. “She is confused, she cannot walk, and she just wants to die, it’s really awful,” says Helms.
“She’s only 60, but she has said to me ‘Covid has killed me’ – meaning it has killed her brain. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Introduction. Neurological Complications of Coronavirus Disease (COVID-19): Encephalopathy. Abstract. The stroke virus? Covid causes hundreds of microclots throughout the lungs (and everywhere else) Could a mass clotting event explain the excess death rate, the hypoxia, the delirium Stories are now appearing of a few youngish people losing fingers, toes or even getting a leg amputated. And strokes have been seen in some as young as 30. Coronavirus, it seems, doesn’t just cause blood clotting, it causes the large and small sort, arterial ones, venous ones, and now microclots, and many of them all through the lungs and other tissues.
This might explain the hypoxia, and also the other cases of organ failure. And while strokes in 33 year olds are still very rare (even in Coronavirus patients) the clotting could be the factor that matters most in the lungs, and in mortality. This also might explain why ventilators are not working too well. COVID 19 Clinical Guidance Summary MIS C Hyperinflammation AKA PMIS. Radiologists sharing CT scans, X-rays in global effort to prevent COVID-19 deaths. Coronavirus symptoms start about five days after exposure, Johns Hopkins study finds. By Jonathan Eichberger /Published March 9. 'Weird as hell’: the Covid-19 patients who have symptoms for months. COVID-19 pathophysiology: A review. Etudes. Thousands Who Got COVID-19 in March Are Still Sick. Editor’s Note:The Atlantic is making vital coverage of the coronavirus available to all readers.
Find the collection here. For Vonny LeClerc, day one was March 16. SARS-COV-2. Intervention.ally. OverTime. Test Test Goose. Far reaching. Viral Health. COVID-19. Pandemic Problems. Robust. Les symptômes, la contagiosité et la période d'incubation.
CoVid-19: Symptomology. Covid-19: Long Haulers.